In my last Biller’s Blog Special Edition: Correcting Invalid Payer Information I reviewed how to properly update patient insurance policy information when encountering an invalid/expired policy. Click here if you missed it and would like to read it now.

If you have received payments from a payer on an invalid policy, you will need to refund those payments.
There are two usual scenarios for refunding of overpayments. Let’s look at both and the steps to enter the refunds in the patient’s account.
1. Most often, office staff becomes aware of an overpayment by receipt of payer correspondence that is requesting the reimbursement of the overpaid funds by check back to the payer. Follow these steps:
Open your Practice Payment Manager and select “New Insurer Payment”. You will create a “zero payment” for the payer indicated.
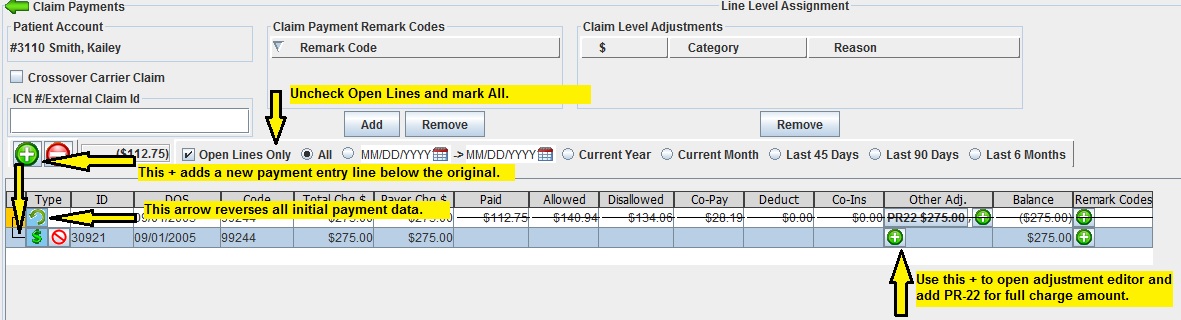
Select “Add Line Level Payment” and enter the patient’s name.
As this screen often defaults to “Open Service Lines” you may need to mark the “All Service Lines” indicator.
Once you locate the service lines that were overpaid, select the green backwards arrow, to reverse the original payment.
Use the green + sign to add a payment line; here you will enter an adjustment of Patient Responsibility (PR) 22-Payment adjusted because this care may be covered by another payer per coordination of benefits. (This reversal and adjustment creates a credit amount on the service line equal to the refund amount.)
Once you have performed the above steps on all overpaid service lines, select “Save”.
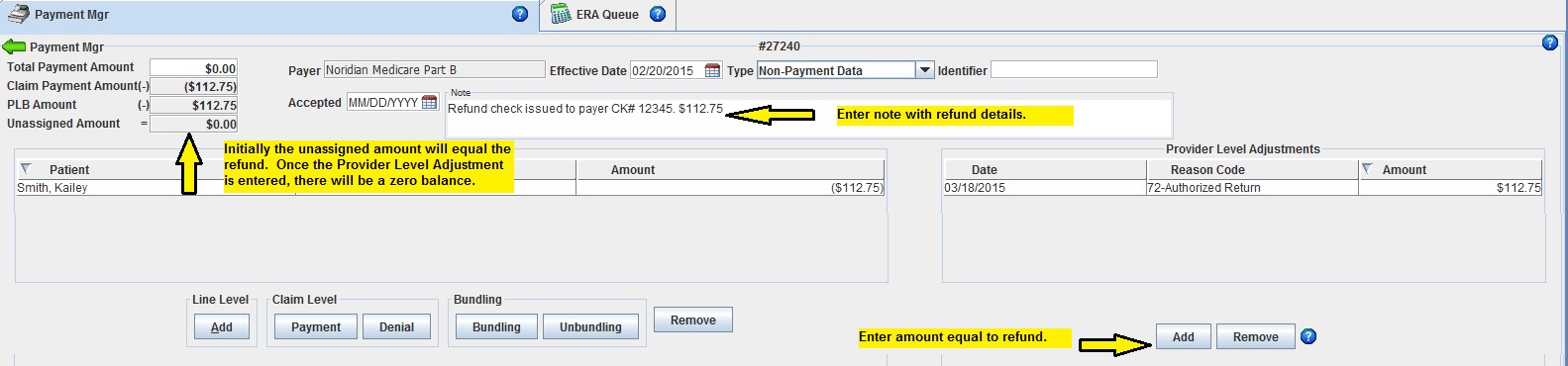
You will be taken to the Claims Payment screen of the Payment Manager. The unassigned amount listed will be equal to the total requested refund amount.
Enter a provider level adjustment equal to the total refund amount. It is helpful to indicate the check #, etc. in the notes section of this screen.
2. Other times, the payer will recoup the overpaid funds on a future claims processing. This process is slightly different for ERA and paper explanation of benefits (EOB).

If this recoupment is received via ERA directly into Iridium Suite, the system will perform the payment reversal automatically and apply those unassigned funds to the newly processed service lines. Typically no user intervention is necessary.
If the recoupment is indicated on a paper EOB, you will follow these same steps as above:
Select “Add Line Level Payment” and enter the patient’s name.
As this screen often defaults to “Open Service Lines” you may need to mark the “All Service Lines” indicator.
Once you locate the service lines that were overpaid, select the green backwards arrow, to reverse the original payment.
Use the green + sign to add a payment line; here you will enter the adjustment indicated on the EOB. It will most likely be Patient Responsibility (PR) 22-Payment adjusted because this care may be covered by another payer per coordination of benefits.
Post remaining payments as indicated on the EOB which will zero out the Unassigned Balance equal to the overpaid recoupment amount.
Hopefully this Biller’s Blog Special Edition has shed some light on the steps necessary to properly post a payer refund. Remember all of this information and more is available at the click of a mouse with the built-in Help Manual.


