Professional rodeo in the US consists of many exciting, but physically dangerous events. Many based on the traditional skills required by cowboys over the years to break horses, round up cattle for branding, cattle herding, etc.
Running your medical practice is surely not physically dangerous, but bad management runs the risk of financial dangers.
Let’s have some fun looking at how lessons from the rodeo relate to your medical office workflow and can help you achieve financial success.
Rodeo Event #1 – Bronc Riding

A successful run requires the rider to stay on the horse for a minimum of 8 seconds.
Winners are determined by the scores based on his and the horse’s performance.
Billing Office Step #1 – Patient Eligibility and Benefit Verification
To successfully collect for services rendered a front desk/scheduler should verify patient eligibility and benefits prior to the scheduled appointment.
Filing claims to the proper payer and collecting appropriate patient responsibilities at the time of service improves cash flow and collection rates of the practice.
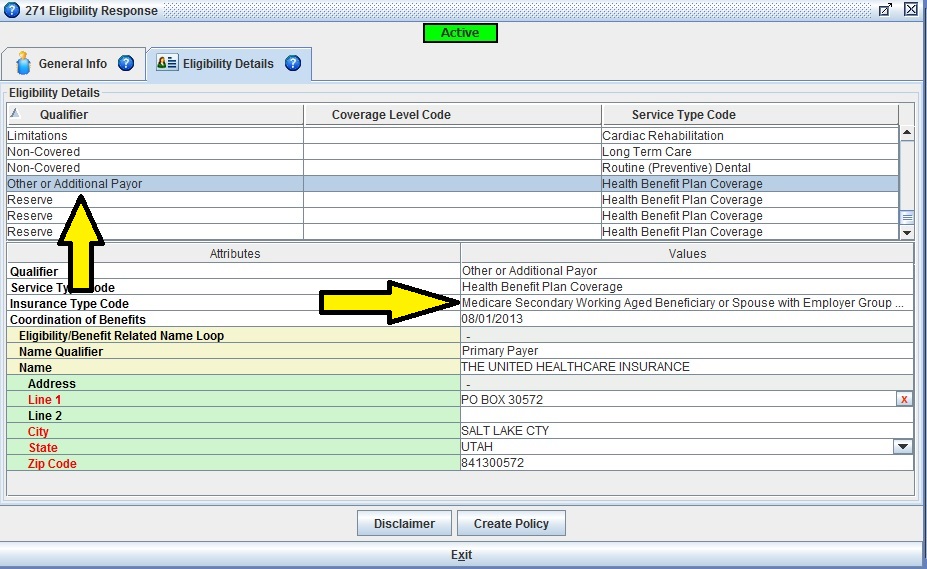
Iridi um Suite practice management software has a built in Real-time Eligibility function. Features include:
um Suite practice management software has a built in Real-time Eligibility function. Features include:
User can send an inquiry to numerous payers with an immediate response
Responses can provide: activity status, eligibility dates, and benefit information
Responses are saved as part of patient account details
A new patient account and/or insurance policy can be created directly from the response.
Rodeo Event #2 – Steer Wrestling

A successful run is when a rider chases a steer, jumps from the horse to the steer and wrestles it to the ground by twisting its horns.
The rider with the quickest time is the winner.
Billing Office Step #2 – Obtaining Service Authorizations
As part of the benefit verification step, the authorization requirements should be obtained as well.
Authorizations can be difficult to obtain and on occasion will be received down to the wire of the procedure. Beginning the process as soon as possible and diligent follow up is a necessary part of this process.
Any services billed without the required approval on the claim will be denied. This provides an unnecessary burden of appeals on office staff and delays payments.
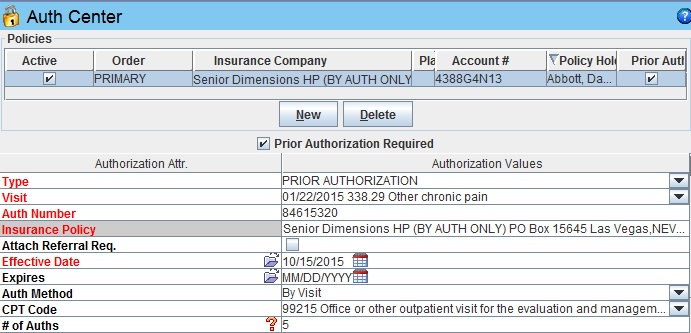
Iridium Suite has a specialized Authorization Management section in the patient chart. Features include:
 Insurance policies are marked if authorizations are required to assist scheduling staff
Insurance policies are marked if authorizations are required to assist scheduling staff
Authorizations are stored/assigned to a specific visit, CPT code and/or treatment course
Authorizations are automatically attached to the appropriate claim /service
As used, the # of authorized units are counted down
Built-in scrubber advises user if authorization is expired or has no units remaining prior to claim submission.
Rodeo Event #3 – Calf Roping

A successful run is when a rider manages to catch the calf with a rope, dismount the horse, and then restrain it by tying three legs together
The rider with the quickest time is the winner.
Billing Office Step #3 – Service Charge Collection

Billers need to avoid denials for exceeding the payer’s timely filing limits. Priority is given to gather charges from charge slips or the code capture function of the electronic medical record.
Time is also allotted for the review of medical documentation for completeness, appropriateness of selected codes and claim accuracy. The thoroughness of this process reduces denials, rejections and audits all which negatively impact the cash flow of the practice.
 Iridium Suite has charge import capability and a built-in claim scrubber. Features include:
Iridium Suite has charge import capability and a built-in claim scrubber. Features include:
Connectivity Clearinghouse: Allows data exchange between billing system and your EMR via HL7 connection. Eliminates need for duplicate data entry.
Built-in Claim Scrubber: Utilizing CCI edits, payer eligibility and authorization check, charges are scrubbed for potential issues and users are warned.
Rodeo Event #4 – Barrel Racing

This is an event whose major emphasis is agility and speed. For a successful run a rider completes a cloverleaf pattern around three 55 gallon barrels.
Variations from the pattern cause disqualification and penalties are issued for knocking barrels.
The winner has the quickest time.
Billing Office Step #4 – Payer Medical Policies
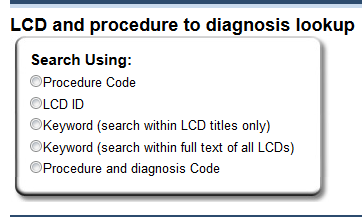
An integral part of your office policies and procedures needs to be based upon familiar knowledge of the commercial payer medical policies and the Medicare national and local coverage determinations.
This knowledge is a valuable tool in ensuring services provided fall under the medical necessity guidelines or that steps can be taken to get additional prior service approvals, avoiding denials. Patients will be able to get the care required and the provider will be reimbursed accordingly.
Custom claim scrubber rules are offered in Iridium Suite. This feature:
Has rules created by IT based upon coding requirements identified by practice
Is able to be assigned practice wide or payer specific
Can suggest a more appropriate “replacement” code, warn of a code conflict, or can auto-generate codes as applicable.
Rodeo Event #5 – Bull Riding

Probably the hardest and most dangerous event, a rider attempts to stay on the back of a large bull for 8 seconds.
Winners are determined by the scores based on his and the bull’s performance.
Billing Office Step #5 – Accounts Receivable Follow Up
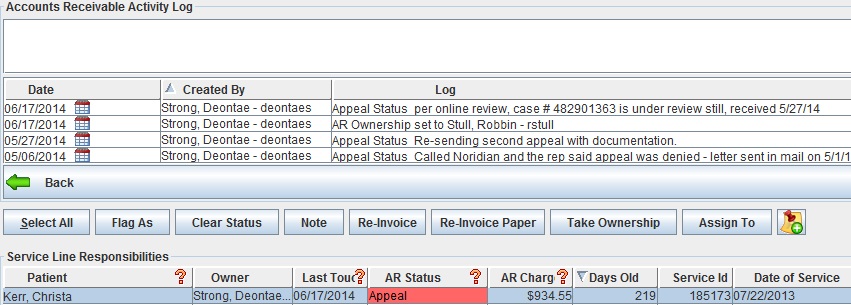
This can often be the hardest and most financially dangerous task in the billing office. If follow up of outstanding charges is let go or mismanaged, this can be the kiss of death for a medical practice. The longer the balances are carried, the less likely payments will be received.
With the specialized Accounts Receivable module in Iridium Suite, keeping on top of your revenue cycle management is easy. Features include:
IQueue : One click evaluates all open payer ARs and highlights those of the highest priority for follow up.
: One click evaluates all open payer ARs and highlights those of the highest priority for follow up.
MyQueue: A queueing system you customize. Your specialized work buckets identify specific ARs for appropriate follow up.
Aging Patient ARs: Aseparate area for all patient balances. It contains all account history, facilitating thorough patient payment communications.

After a long day at work or the rodeo, nothing’s better than a hearty meal.
Get recipe for: Rachael Ray’s Cowboy Chili and Baked Bean Pot
Getting authorizations can feel like wrestling a steer and making a payer to overturn an inappropriate denial maybe like riding that wild bull. A practice management system that gives you the upper hand can get you through the billing rodeo a lot less beat up. Contact us today for a free demo!


