Last month I wrote about common clearinghouse claim rejections and how to prevent them.
 If you missed it, click here.
If you missed it, click here.
Not a Shavara customer yet? Get your free demo today!
In this edition of our Biller’s Blog, we will look at payer level rejections.
Timely payer reimbursements are crucial to the cash flow of any medical practice or billing service. By reducing or even eliminating payer rejections, this significantly improves the turnaround time for your payments.
The payer level rejections are usually based on their pre-processing claim edits.
Based on rejection data from the clearinghouse, the items below represent three common reasons.
1. Invalid subscriber/patient name, date of birth or identification number or policy not in effect at time of service.
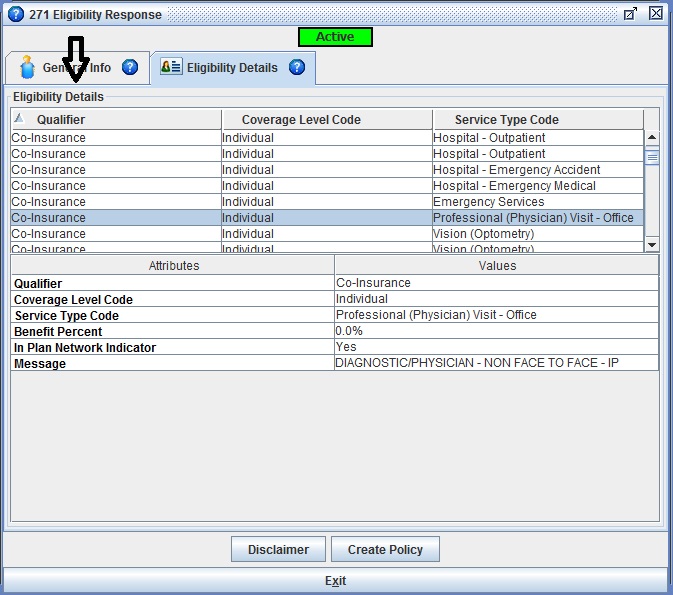
Patients do not always remember to provide their most up to date insurance information. It is possible to verify the information quickly by using the built-in Real Time Eligibility inquiry function. The policy will show as active or inactive.

Active policies will show details such as: patient identification #, patient date of birth, subscriber name if different from patient, and often other benefit details like deductible, co-insurance and out of pocket amounts.
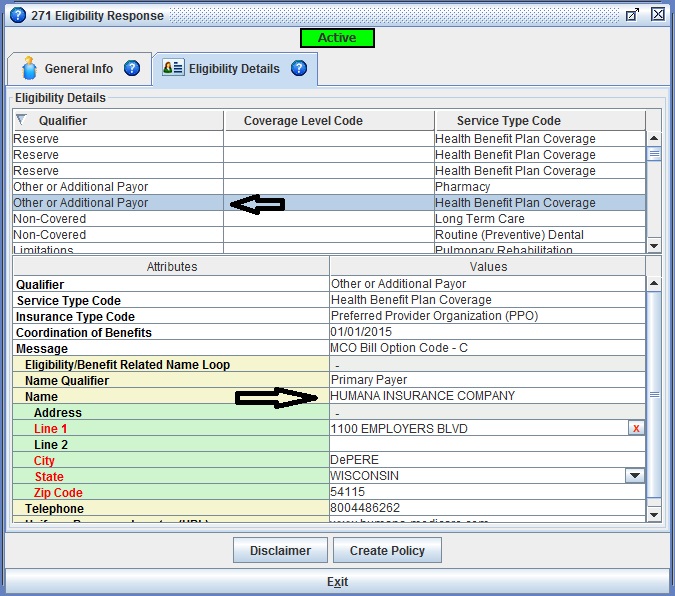
In the case of Medicare beneficiaries, they can be confused that when enrolling for a Medicare advantage/replacement plan they should no longer provide their traditional Medicare card as coverage. The RTE response for Medicare confirms they are active, but in the details you can find the information about the Medicare replacement plan under “Other or Additional Payer”.
2. Required professional modifier not on claim.
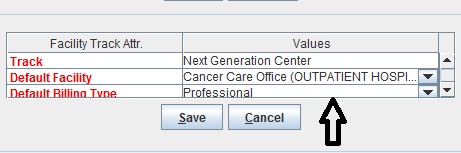
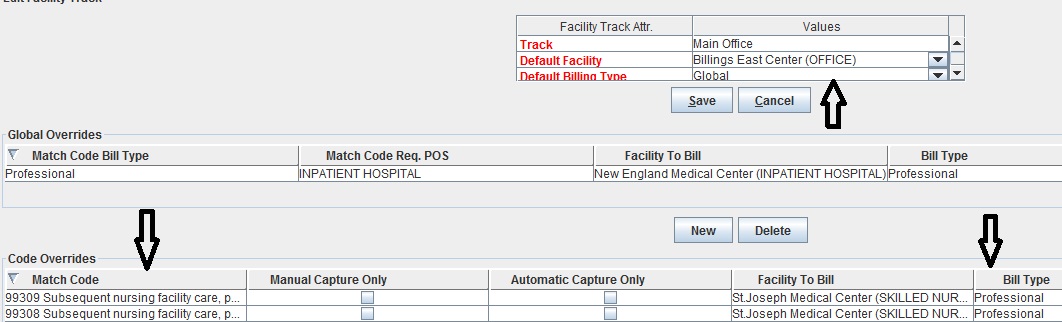
If you are billing the “professional” component or “technical” component only of a global procedure code, it is imperative the proper modifier is attached to the service line. A 26 indicates professional and TC indicates technical. By setting up your practice facility as a “professional” or “technical” provider, Iridium Suite will analyze the codes captured and for all applicable codes add the appropriate modifier.
You can even you’re your practice set as global billing and add “exceptions” where you will only bill the professional or technical component. This automation prevents users from forgetting when the modifiers should be applied.
3. Adjudication or payment date incorrect.
This is the one that is only somewhat preventable. The typical offender is Medicare as a primary payer via ERA when combined with a secondary electronic claim. Often Medicare will transmit an ERA file on one day (example 5/1/2016) but have the data marked as effective on a later day (example 5/3/2016).

If a practice submits the electronic secondary claim before the effective date 5/3/2016, it gets rejected. The rejection message reads something like this: Adjudication or Payment Date is incorrect. Value for date or start period date is expected to be a date earlier than the Transaction Creation Date.
There are two options to deal with these rejections:
1. Wait a day or two after receiving a Medicare ERA to submit the secondary claims or check the effective date to know for sure when it is safe to send them.
2. Transmit claims as you regularly do, but check every day for rejections. Any that come across with the above message can just be re-invoiced right from the Electronic Claims Queue.
Check back next month for Part 3: Denials


