Almost daily there is a news story about billing fraud in healthcare. There are those providers and practices that knowingly participate in fraudulent billing practices. The rest of the industry makes valiant attempts to follow appropriate practices.
We all know, as humans we make mistakes. Honest  mistakes are not the same as fraud, but if not addressed, can prompt a payer audit. Practice administrators never want to see an audit notice from a payer.
mistakes are not the same as fraud, but if not addressed, can prompt a payer audit. Practice administrators never want to see an audit notice from a payer.
In this series of billing blogs, I want to go over some common mistakes and ways you can utilize features in the advanced billing software, Iridium Suite, to minimize mistakes and identify potential billing issues.
The first issue I want to discuss is bundled codes. As we all know, billing rules change frequently. Our built-in scrubber features CCI edits, 10 and 90-day global surgical period rules, requirements for add-on codes, etc.
Let’s look at the Built-in Customized Scrubber
With CCI edits, most claim checking programs can only compare codes billed on same date of service, there are instances when codes are still considered bundled even if done on different dates of service.
One radiation oncology billing example for 2017 is the inclusion of code 77280 in the reimbursement of code 77301. In 2016, there was waffling on the ruling. First it was included, and then it was excluded if it represented the verification simulation prior to treatment. The latest publication from CMS, puts it back in. It’s enough to make your head spin.
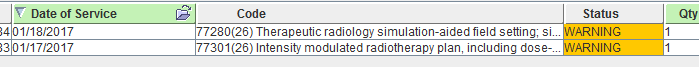
By using a customized scrubber rule for this specific circumstance, the system can identify a patient that has been billed 77301 and then subsequently the 77280. A warning is given to the user allowing the opportunity to review the code entry.
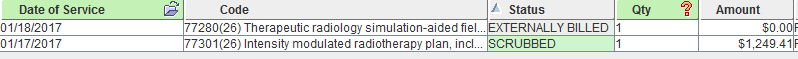
Iridium Suite has an additional feature that allows a user to mark a code like that “Externally Billed”. This keeps the service on file as a reference only with a $0 charge.
If CMS were to overturn their ruling retroactively, you can find those services, mark them “Bill Internally”.
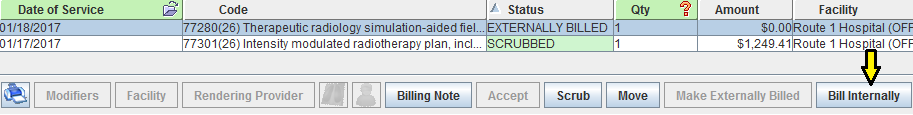
Then file the services.By using a custom scrubber rule that can look beyond a single date of service, you have avoided billing a code that might:
Be reimbursed in error requiring a payer refund
Denied causing AR follow up to write off
Be flagged as fraudulent billing initiating a payer audit.
 Before it’s too late, learn more with a
Before it’s too late, learn more with a
free Iridium Suite Practice Management Software demonstration.


