Click Here to Learn to Think Catalysis
Let’s be honest, in most healthcare businesses we are doing more and more with less and less staff. The end of the day/week is here before you know it. That list of tasks, stack of papers and inboxes still full of unopened messages are still there.
This common scenario often drives us to focus more on the “revenue” than the “cycle” in our Revenue Cycle analysis. See our Medical Billing Blog: We Should Focus on the Cycle as Much as the Revenue.
The amount of money collected from both payers and patients is obviously a valid point, but we should take the time to look at how and when it is collected and why it’s not. In this issue, we will analyze the patient responsibility collection process.
issue, we will analyze the patient responsibility collection process.
How and when do you collect patient money?
Do you bill after services, at point of service, provide responsibility estimates, establish payment arrangements upon initial visit? The best financial plan for your office is actually a combination of all of these. Here is how you can implement:
1. When office staff members are verifying patient eligibility it is important to also get the details of the patient benefits. Key benefit elements are:
a. What is the annual deductible and amount remaining?
b. What is the benefit coverage percentage (example: 70%, 80%, 90% etc) once deductible is met?
c. Is there an out of pocket maximum? If so, what is the amount remaining?
d. Are there services subject to flat co-payment amount (example: office visits, diagnostic testing, outpatient procedures)?

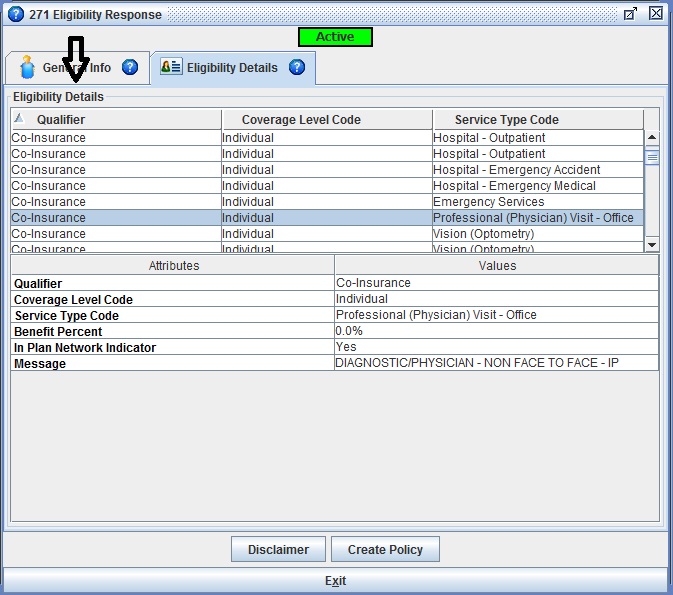
Advanced medical billing software like Iridium Suite, provide built-in Real Time Eligibility (RTE) inquiry functionality. Many payers provide detailed benefit information with the eligibility results.
2. Point of service collections often apply to the services subject to the flat co-payments. It has become common for patients to be aware of these requirements, but it is courteous to advise patients prior to their service. A great time to accomplish this is when the patient is contacted to confirm the upcoming appointment.
3. If your policy is to bill after services, you should generate an estimation of the patient’s responsibility and provide that information as soon as available.
4. For both 2 and 3 above, once you have begun the financial discussion with the patient, any issues the patient anticipates meeting their responsibility can be brought to light. This gives each party the appropriate forum for working out payment plan arrangements when payment in full in not viable.
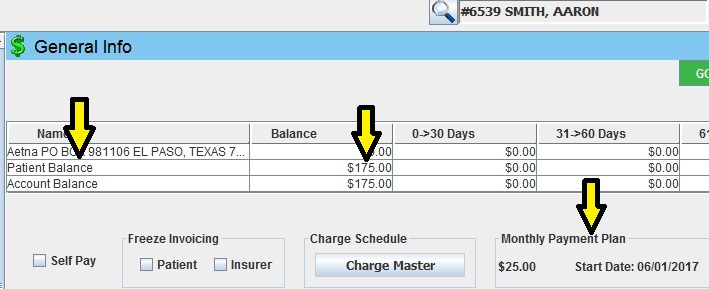
Iridium Suite provides an easy way to indicate a Payment Plan arrangement for your patients.
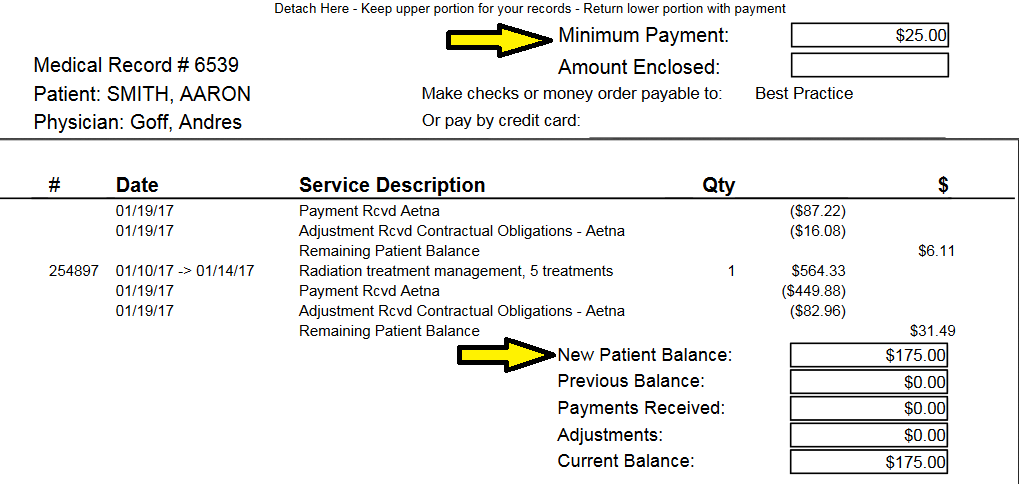
It utilizes this information when generating patient statements. It will reflect the patient total balance, but clearly indicates the expected payment plan amount.
to our Medical Billing Blog to get the next part in this series: A Better Analysis of the Revenue Cycle-Payer Uncollectables.


