Why is payer money not collected?
It is estimated that 30-40% of denials are due to front-end registration and eligibility issues. If billing staff are diligent with the patient benefit verification steps from our last Medical Billing Blog: A Better Analysis of the Revenue Cycle-Patient Collections, you should be able to reduce that percentage to almost 0%.
Another co mmon denial cause is authorization issues, usually lack of authorization. As part of the benefit screening for patients, it is imperative authorization requirements are also checked. Even if you receive the proper approval, you must be sure that it is included on the claims.
mmon denial cause is authorization issues, usually lack of authorization. As part of the benefit screening for patients, it is imperative authorization requirements are also checked. Even if you receive the proper approval, you must be sure that it is included on the claims.
Iridium Suite is designed with several authorization “safe guards” to ensure appropriate authorizations are attached to services.
1. When adding the insurance to a patient account, users indicate on the account for any payer policies that require authorization.
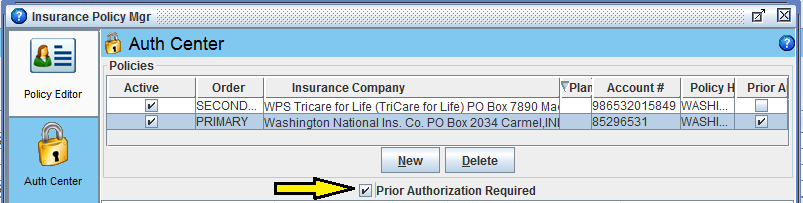
2. The authorization is entered into the Authorization Center. By completing all the details accurately it ensures the software attaches the correct one to the claim in case you have multiple authorizations for one patient.
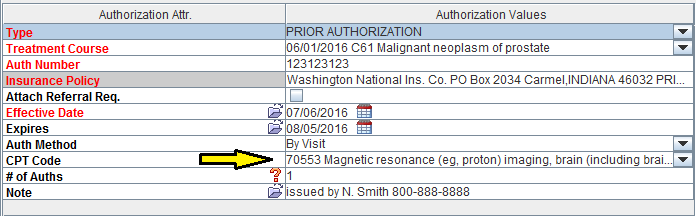
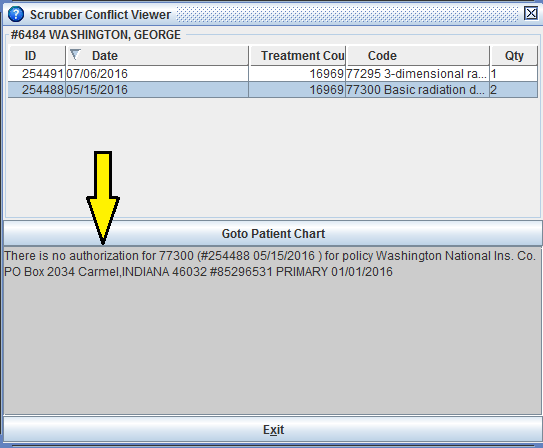
3. The built-in Claims Scrubber Aautomatically checks accounts marked with “Prior Authorization Required” as charge are captured. It will warn the user if an appropriate authorization is not on file. This prevents submission of a claim with inaccurate or missing authorization information.
One of the best defenses against un-collectable payer revenue is analyzing denial data. Iridium Suite has several reports designed to identify payer issues. Let’s see how to use two to drill down into specific issues:
First, I run the Denial > Reason Code Summary Report. Reason codes are returned on the explanation of benefits and represent a standard list of informational codes describing the reason for any payment adjustment. We all are familiar with code -45 as it is used for the contractual write-off.
In the results, I look for outliers, codes that seem to have much higher than average frequency.
|
Reason Codes |
# of Denials |
|
29-The time limit for filing has expired. |
1 |
|
45-Charges exceed your contracted/ legislated fee arrangement. |
2 |
|
50-These are non-covered services because this is not deemed a 'medical necessity' by the payer. |
30 |
Then I can run a detail report for code -50 to see if this is an issue with a specific CPT, provider, payer, etc.
|
Payer |
Service Date |
CPT Code |
|
Beech Street |
2/1/2015 |
99215 |
|
Beech Street |
10/15/2016 |
99203 |
|
Noridian Medicare |
11/17/2015 |
77338 |
|
Noridian Medicare |
11/17/2015 |
77338 |
|
Noridian Medicare |
11/18/2015 |
G6015 |
|
Noridian Medicare |
11/18/2015 |
G6015 |
Using this analysis you can identify common issues and resolve to eliminate these denials.

If you are not a current Iridium Suite Practice Management Software user, then contact us today for your free demo!


